Amoxicillin in pediatric practice: Amoxicillin / clavulanic acid (amoxiclav) is an inhibitor—protected beta-lactam antibiotic that has been successfully used in clinical practice for more than 30 years. During this time, numerous data have been accumulated on the use of the drug in various bacterial infections: the scientific literature presents the results of several hundred randomized clinical trials on the efficacy and safety of Amoxil. At the same time, the largest share is made up of publications concerning the use of the drug for respiratory system infections in children. However, despite a long and comprehensive study, there are new questions related to the use of amoxicillin. They relate in most cases to the mode of use of the drug — the ratio of components in the drug, dosage form, single dose, frequency of use, duration of treatment, etc. The emergence of new controversial issues is associated with a change in the sensitivity of infectious agents to antibacterial drugs.
Several dosage forms of Co-amoxiclav (coated tablets, soluble tablets, powder for the preparation of oral suspension, powder for the preparation of an injectable solution) with fundamentally different variants of the ratio of active substances are currently presented on the world pharmaceutical market (2:1, 4:1, 7:1, 14:1, 16:1). Naturally, a practical doctor, especially a pediatrician, has a number of questions:
- what kind of drug containing Co-amoxiclav should be prescribed to a specific patient?
- what form of drug should I choose for a child?
- in what mode should the drug be used?
For correct answers to these questions, both information about the drug itself (efficacy, safety, pharmacokinetics, etc.) and knowledge in the field of clinical microbiology (sensitivity of infectious agents to the drug) are required.
Amoxicillin is a derivative of another antibiotic — ampicillin, together they make up a subclass of aminopenicillins — semi-synthetic antibiotics from the penicillin class. Like other β-lactams, aminopenicillins have a bactericidal effect by inhibiting the synthesis of the bacterial cell wall. Aminopenicillins are active against gram-positive cocci (streptococci, pneumococci, enterococci, penicillin-sensitive staphylococci), gram-positive bacilli (listeria, Corynebacteria), gram-negative cocci (neisseria), some gram-negative bacilli (Hemophilus bacillus, Helicobacter, individual bacteria of the intestinal family), many anaerobic bacteria, spirochaetes, actinomycetes. The activity spectra of amoxicillin and ampicillin practically do not differ, but amoxicillin has significantly better pharmacokinetics, which provides higher and stable concentrations in blood and tissues. With oral use, the bioavailability of amoxicillin is more than 75% and does not depend on food intake, whereas ampicillin’s bioavailability is less than 40% and significantly decreases with simultaneous food intake.
Amoxicillin in pediatric practice – so, the obvious disadvantage of aminopenicillins is their complete vulnerability to any β-lactamases. Currently, aminopenicillins have lost their importance in the treatment of many infections, in particular, caused by staphylococci and bacteria of the intestinal family, due to the formation of resistance in pathogens, primarily as a result of the production of beta-lactamases, which leads to enzymatic inactivation of antibiotics. Also of fundamental importance for clinical practice is the increase in the proportion of β-lactamase-producing strains of Haemophilus influenzae in recent years.
Amoxicillin in pediatric practice
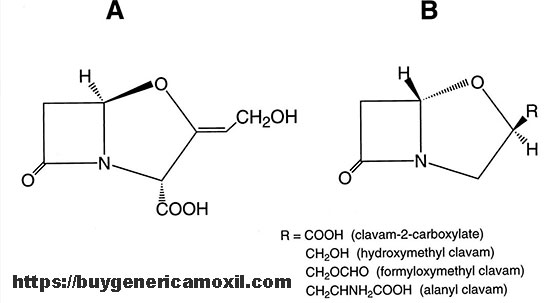
An effective method of overcoming bacterial resistance caused by the production of β-lactamases is the use of a combination of antibiotics with β-lactamase inhibitors — salts of clavulanic acid, sulbactam, tazobactam, etc. Inhibitors by chemical structure are also beta-lactams, which do not have their own antimicrobial activity (or have limited activity), but neutralize bacterial enzymes by “self-sacrifice”, thus protecting the antibiotic from hydrolysis. The use of a combination of penicillins or cephalosporins with an inhibitor leads to the restoration of antibiotic activity against many strains of bacteria with secondary resistance due to the production of β-lactamases: methicillin-sensitive staphylococci, H. influenzae, Moraxella (M.) catarrhalis, many intestinal bacteria, etc. But, in addition, the combination of amoxicillin with clavulanic acid has activity against a number of gram-negative microorganisms with natural resistance to aminopenicillins (due to stable production of β-lactamases): Klebsiella spp., Bacteroides spp. and some others. Both components of Co-amoxiclave create high concentrations in many organs and tissues where the bactericidal effect of the drug is realized.
Due to the steady increase in the number of resistant strains of bacterial pathogens, the structure of prescribed antibiotics has been changing in recent years. A pharmacoepidemiological study conducted in the USA is indicative, in which the use of antibiotics in outpatient settings for respiratory infections in 1995-1996 and 2005-2006 was compared. The total number of prescriptions of antibacterial drugs has decreased over 10 years, which is obviously due to the introduction of universal vaccination against pneumococcal infection for young children. In particular, the frequency of penicillin prescribing as a whole decreased by 31%.
But if amoxicillin was prescribed significantly less often (by 33%), then Co-amoxiclav — a little more often (by 14%). In France, amoxicillin/clavulanate was prescribed in children’s emergency departments in 2005-2009 in 50% of the total number of cases of antibiotic prescribing for respiratory infection. Analysis of data on the use of antibiotics in outpatient settings in 33 European countries showed that over 13 years (1997-2009), the frequency of Co-amoxiclave use in most countries increased — on average by more than 2 times. Pharmacoepidemiological studies conducted in recent years in Canada also indicate an increase in the use of inhibitor-protected penicillins, primarily Co-amoxiclav.